Education
Religion
Domicile: Urban Work: Govt. School Teacher
Languages known
Reason for Referral
Informants
Chief Complaints:
• Forgetfulness
• Behavioral issues and inability to do daily chores
• Self-talk and laugh
• Decreased sleep Since 3 years
• Seizures
• Wandering behavior
Brief History:
History of Present Illness:
She cannot remember which thing is kept where in the house, like her cupboard or what all ingredients are required to cook a meal. She also does not know how to count money. She needs to be instructed every small detail to do a task. For an example, every morning she has to be told
Sometimes the patient
Past Medical and Psychiatric history
The patient is undergoing treatment from neurologists in past 3 years. After the accident the patient was taken to
There she gained consciousness, underwent further MRI scans and was later discharged after over a month. She could not walk by self for next six months and would hardly talk to anyone for the next one year. Physically she had recovered well until on 26th May 2016 where she had multiple seizures and was admitted for 2days in
Family History:
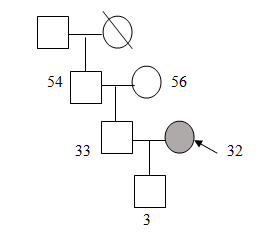 |
| Family Genogram |
The client lives in a joint family with her husband, her in-laws and her husband’s grandfather. She has a 3 year old son. Her family is supportive to her illness, especially her husband. Her mother-in-law takes care of the family
Personal History:
The client was born with a full term normal delivery with
Mental Status Examination:
General appearance and behavior: General appearance was well kept and tidy, age appropriate, head and neck was covered with a
Attitude towards examiner: She was not cooperative towards examiner, she was distracted and inattentive.
Speech: Her speech was comprehensible and spontaneous. Excessive talkativeness and pressure of speech was observed
Mood and Affect: Subjectively the mood was reported to be normal. Verbatim: “
Objective mood: It was observed to be
Thought:
Stream of Thought: Flight of ideas was present.
Content of thought: Suspiciousness was present.
Possession of thought: No abnormalities
Perception: No perceptual disturbances were found.
Cognitive functions:
Orientation: Patient was not oriented to time, place and person.
Attention: Attention was
Memory: Immediate, Recent and remote were found to be impaired.
General Information: General intelligence was found to be below average.
Abstract Thinking: Abstraction ability was found to be at conceptual level based on the tests of similarities and differences.
Judgment: Personal, test and social judgment was intact as the client showed
Insight: It was present at Grade I (Complete denial). She said – “I am not sick, nothing is wrong with me”.
Reason for Psychological assessment- To test whether the client has some impairment in her Neuro-cognitive functioning.
Test Administered
Luria-Nebraska Neuropsychological Battery- To evaluate quantitatively and qualitatively any neuropsychological and cognitive deficit.
Test Findings
Luria-Nebraska Neuropsychological Battery:
The critical level on the basis of age of the client and her educational qualifications is 49.19. Significant elevations are considered = 3 Scores from the critical level.
Clinical Scales: 12 scales were above the critical level, namely C2, C3, C4, C6, C7, C9, C10, C11, S1, S2, S4 and S5 denoting rhythm, tactile, visual functioning, expressive speech, writing, arithmetic, memory, intellectual processes, intermediate memory, pathognomic, left hemisphere, Profile Elevation and impairment respectively.
Localization scales: there are 6 scales above the critical level, namely L1 (left frontal), L2 (Left Sensorimotor), L3 (Left-Parietal Occipital), L6 (Right Sensorimotor), L7 (Right Parietal-Occipital) and L8 (Right Temporal).
Factor scales: there are 13 scales above the critical level, namely E1 (Simple Phonetic Reading), E2 ( Word Repetition), E3 (Reading Polysyllabic Word) RE1 (reading Complex Material), RE2 (Reading Simple Material), W1 (Spelling), W2 (Motor Writing Skills), A1(Arithmetic calculations), ME1 (Verbal memory), ME2 (Visual and complex memory), I1 (General verbal intelligence), I2 (Complex verbal arithmetic) and I3 (Simple verbal arithmetic).
The scores have been found to be indicative of inability to perceive tonal qualities and their
Other impairments are found in speech and motor moments,
Ability to copy letters and words as well as write it from dictation is impaired. Client is unable to solve arithmetic calculations. There is inability to recall words visually and orally (short term memory) and to memorize verbal and visual information and integration of visual memory with motor skills. Inability to verbally describe, define and analyze information or to formulate and solve difficult verbal arithmetic problems has been found in addition with impairment of simple arithmetic skills.
Summary of Test Findings
The patient’s cognitive functioning was assessed using Luria- Nebraska neuropsychological battery, among the Clinical scales, her highest score elevation is above critical level on scales of rhythm, tactile, visual functioning, expressive speech, writing, arithmetic, memory, intellectual processes, intermediate memory, pathognomic, left hemisphere, Profile Elevation and impairment respectively denoting impairment in writing, speech and failure to comprehend instructions.
Inability to retrieve from short term memory and significant time delay has also been observed. Localization scales: there are 6 scales above the critical level, i.e. of left frontal, Left Sensorimotor, Left-Parietal Occipital, Right Sensorimotor, Right Parietal-Occipital and Right Temporal. On Factor scales 13 scales above the critical level, namely Simple Phonetic Reading, Word Repetition, Reading Polysyllabic Word, reading Complex Material, Reading Simple Material, Spelling, Motor Writing Skills, Arithmetic calculations, Verbal memory, Visual and complex memory, General verbal intelligence, Complex verbal arithmetic and Simple verbal arithmetic.
It shows the client’s inability to comprehend both a relationship expressed verbally and then to use this relationship to understand some circumstance or carry out some behavior, inability to solve arithmetic calculations, involves recalling a list of words presented visually and orally which requires short term memory. The client also has an inability in repeating stories and words associated with pictures, interpreting and verbally describing pictures, analyzing stories, defining words, formulating and solving relatively difficult verbal arithmetic problems. The results are associated with poor emotional control, insight and understanding, indicative of poor understanding of non-verbal cues.
Clinical impression:
According to chief-complaints, history of present illness, mental status examination and test findings, the client has diffused impairment in fronto-parietal and temporal lobes.
Management plan:
Cognitive retraining
Pharmacological treatment
Psycho education
Behavioral modification
More: Student With Specific Learning Disabilities Case Study Psychology
Mixed Learning Disorder Case Study Using Malin’s Intelligence Scale for Indian children
